For healthcare providers, getting their medical claims approved is critical to their survival in the industry and the well-being of their employees. But it’s a cause of serious concern as medical claims processing is quite complex due to the involvement of multiple variables. For instance, the billing process itself can take weeks or even months at stretch depending on the complexity of the case. Quicker submission of claims and approvals are only possible when the internal workflow of the practice is in perfect sync with the external elements such as clearinghouses and claims processing vendors.
The following tips would help care providers with an effective medical claims billing process to power its revenue wheel.
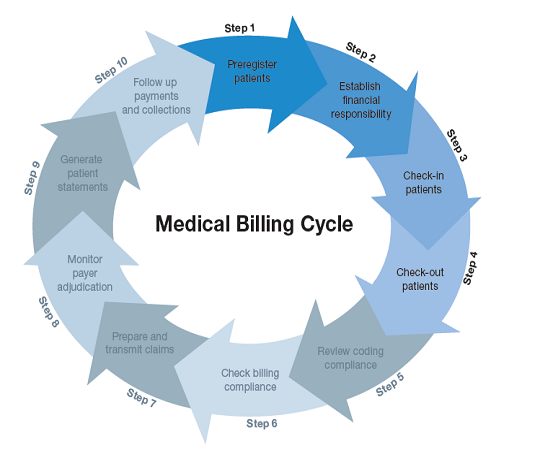
A proven workflow in place is the first step to an unhindered revenue stream for providers. It should be an all-encompassing approach with step-wise guidance for all employees to ensure better cash inflows. Providers must communicate their expectations from the patient about the financial terms of the treatment including co-pays. They should muster the relevant information about the patient to file the claim. The providers should venture beyond just collecting the details and conduct a thorough verification to check their authenticity. Among the items to be verified, the patient’s insurance card and their eligibility for the coverage sought are critical.
Employee the best people
Providers can either seek the services of a specialized insurance services provider to take care of their medical claims processing or train their in-house teams to do the job. If they opt for the latter, the training should focus on acquainting the individuals with the company protocols and empowering them to master the process. The claims processing team should be in tandem with the billing department to facilitate an unhindered flow of relevant information and other filing requirements to expedite the submission process.
Attention to detail
Any wrong information in the claims form can lead to the denial of the claim and thus, maintaining the utmost caution is imperative. Incomplete information must be identified and rectified before the form is submitted to the insurer. Also, it’s critical to ensure that the claim is submitted to the right payer. Providers should bear in mind that moving the file back and forth will lead to multiple resubmissions that not only delay payments but also carry the risk of the denials.
Fine-tuning the process
This should be a regular practice of the management to achieve improved claims approval rate in the future. Issues impacting the billing process should be identified and addressed adequately. The management must delve beyond the overall payment or denial numbers and analyze and improve the efficiency of the process. For this, there should be suitable KPIs in place along with the use of a maturity table to gauge their position against industry leaders. Care should be taken to ensure complete adherence to regulatory compliances.
Flawless medical claims processing is a prerequisite for the financial health of practices and it calls for proactive billing procedures to realize increased cash flow, efficient operations, and better patient experience. If practices find it overwhelming to manage such an elaborate process, seeking the help of a professional medical billing consultant firm can ensure the best results for them.
Leave a Reply